













St. Paul’s Hospital is an acute care hospital located in downtown Vancouver, British Columbia, Canada. It is the oldest of the seven health care facilities operated by Providence Health Care, a Roman Catholic faith-based care provider. St. Paul’s is open to patients regardless of their faith and is home to many medical and surgical programs, including cardiac services and kidney care including an advanced structural heart disease program. It is also the home of the Pacific Adult Congenital Heart Disease unit. It is one of the teaching hospitals of the University of British Columbia Faculty of Medicine.
The original St. Paul’s Hospital was founded in 1894 just eight years after the incorporation of the City of Vancouver by the Sisters Of Providence who (from their base in Montreal) founded schools, hospitals and asylums all over North America and other continents.
The 25-bed, 4-storey wood frame building cost $28,000. It was designed and constructed by Mother Joseph of the Sacred Heart and named after the then-bishop, Paul Durieu of New Westminster.
Mother Mary Fredrick from Astoria, Oregon was the first mother superior and administrator to lead its charge. In keeping with the philosophy of the Sisters of Providence, the new hospital was founded on the pledge of providing compassionate care for everyone in need – tested by a surge in Vancouver’s growth brought on by the Klondike gold rush in the 1890s.
St Paul’s became one of the first hospitals with their own X-Ray machine in 1906 and opened its School of Nursing in 1907.
In 1912, the original building was demolished and replaced with a new structure to accommodate 200 patients at a construction cost of $400,000.
In 2010, the hospital established Angel’s Cradle, the first modern Baby hatch in Canada where mothers could anonymously provide their newborns to the hospital rather than abandon them elsewhere. Thirty seconds after a baby has been placed inside the modern version of a ‘foundling wheel’, a sensor alerts emergency staff. A social worker contacts the Ministry of Children and Family Development which then assumes responsibility for the baby. In its first five years, two healthy babies had been placed in the baby hatch.
St. Paul’s Hospital is listed on the City of Vancouver’s Heritage Register category “A” but is not a designated heritage building and is not protected by legal statute.
In the 21st Century, there has been ongoing advocacy for redevelopment of the facility. A redevelopment plan was drafted in 2010. In 2012, Premier Christy Clark said at the hospital that business case and development plans would be completed in order to begin construction in 2016.



Enjoying these old commercials and content? The best way to support the channel is to go to my eBay store, Obsolete Treasures, which features lots of vintage items. You’ll find all sorts of cool things there, including trucker hats/baseball caps, old electronics/stereos/computers/video games, unique jackets, ephemera, and other weird/interesting items from the past (and some newer items that might even be useful). In addition to the sale price, I will receive a commission if you purchase from my store using this link: https://ebay.us/kMTuOX

Autism and ADHD have long been seen as two distinct forms of neurodivergence. But what if they overlap? The term AuDHD has emerged to name this experience, offering validation and bringing clarity to patterns of thought and behaviour that might once have felt confusing or contradictory.
At Leone Centre, we often meet people who have spent much of their lives trying to “make sense” of themselves. They may have been told they are too much, not enough, too sensitive, too intense or too distracted.
Yet what if those very traits are not deficits, but expressions of a different kind of perception, one that deserves listening, not managing?
What happens if we look past those labels? What if, instead of fitting ourselves into categories, we approach these experiences with compassion and curiosity? Often, what emerges is a richer story: the layered, nuanced reality of minds that hold both ADHD and autism, and the humanity that lives beyond any one diagnosis.
AuDHD is not an official term. It’s a word that has emerged from lived experience, from people searching for a language that feels closer to the truth of who they are. It points to the meeting place of autism and ADHD, describing two ways of being once thought to be distinctly separate.
Until 2013, it was not possible to be diagnosed with both ADHD and autism. Systems demanded a choice and one explanation over another. Imagine what that meant for the many who lived with both? Their stories trimmed to fit whichever description seemed most pressing at the time.
Clinically, autism and ADHD are diagnosed separately using DSM-5-TR or ICD-11 criteria, and co-diagnosis is now permitted.
Today, AuDHD offers a bridge that emerges from lived experience, not from textbooks, but from people searching for words that feel closer to the truth. It acknowledges that some people don’t fit neatly into one box or another, that their reality is woven from both to varying degrees. With growing awareness, space is opening for a more balanced approach to research and support that hadn’t been pursued before.
Understanding this overlap is not about collecting labels, but about giving a voice to the challenges and triumphs of a different way of perceiving the world. What possibilities open up when we stop reducing people to categories and begin to notice the richness of their lived experience?
With the ambiguity surrounding AuDHD, many may lean towards doubting their experience as an isolated one. But the statistics tell a different story.
You may be surprised to find that:
Awareness shifts the story. Instead of self-doubt, it can bring a sense of recognition: you are not alone, and you are not an outlier. It also reminds us that no two experiences are identical.
One of the reasons many neurodivergent individuals might question whether they have both autistic and ADHD traits is how we associate attention with either.
In ADHD, the “AD” stands for “attentional deficit”. This can often lead to the assumption that having ADHD translates as an inability to pay attention. In reality, many ADHDers don’t lack attention but experience it differently. They often show interest-driven attention, experiencing periods of hyperfocus, intense and sustained concentration on highly stimulating or rewarding tasks. For many with ADHD, attention is more like sunlight through leaves: scattered and shifting, being pulled in multiple directions. And yet, when something truly resonates or captures interest, they can drop into hyperfocus so completely that time itself seems to bend. Hyperfocus is not unique to ADHD, but it tends to occur more frequently and more disruptively within ADHD populations.
For autistic individuals, focus can be so complete that shifting away feels like loss. Autism is often linked with sustained, deeply focused attention. This can sometimes be so immersive that external circumstances fade into the background. Shifting attention can be difficult, especially when tied to a special interest or when sudden changes in the environment require adaptation.
On the surface, these two portraits may appear distinct. If we look closely, we see the echo: both autistic and ADHD individuals can experience hyper-attention. This crossover can feel confusing, or it can feel like recognition. It tells us something important: the capacity to focus does not cancel out ADHD, just as struggles with focus do not cancel out autism.
AuDHD is not about confinement in a label, but about validation that the overlap itself is real, and that the lives shaped within it are no less whole or worthy of understanding.
When autism and ADHD meet, the result isn’t double the difficulty; it’s a unique choreography of strengths and struggles.
No two AuDHD experiences are the same. Each is a distinct rhythm — a personal constellation of perception and energy.
For many people with AuDHD, recognition comes late, if at all. Some are seen as fitting only one category, while others are misunderstood entirely or dismissed as ‘too anxious’ or ‘too sensitive’’ When their experiences don’t seem to align neatly with either autism or ADHD, they may turn the doubt inward: Maybe I’m just not trying hard enough. Maybe I should know how to function by now.
The cost is often invisible. A quiet erosion of self-trust, with real consequences. It may prevent someone from seeking support altogether, leaving them to carry the belief that they either don’t need help, or worse, don’t deserve it. And when support is offered but focused only on ADHD or only on autism, it may not fit. Sometimes, it even amplifies existing struggles, leaving people feeling more unseen.
The impact of this lack of recognition can include:
Language matters because it shapes how we see ourselves. Language like AuDHD doesn’t fix everything but can open doors: it allows people to name their experience, reclaim their story and seek the kind of support that honours the whole of who they are.
At Leone Centre our focus is not on fixing, but on understanding. Neurodivergence is not a problem to be solved, but a reality to be honoured. For those with AuDHD, therapy can be a space to move beyond labels and into a deeper exploration of what it means to live fully and authentically.
Neurodivergent-affirmative therapy shifts the emphasis from clinical assessment to human connection and practical support. It recognises the complexity of living with both autism and ADHD, and creates space for the ways they converge in everyday life. A psychotherapist’s role is to accompany rather than correct, to listen with curiosity, and to adapt their approach to the unique needs of each individual.
In therapy, this translates to:
Therapy, in this sense, becomes a collaboration: a place where challenges are acknowledged, strengths are celebrated, and a fuller story of self begins to unfold.
When one or both partners have AuDHD, differences in communication, sensory needs, or emotional rhythms can create misunderstandings. Couples therapy provides space to reconnect and better understand each other.
Focus areas include:
Whether both partners are AuDHD or one is neurotypical, therapy can help to build balance, compassion, and deeper connection.
Moving from tolerance to celebration begins with how we show up in everyday life. For individuals with AuDHD, the difference is felt in whether they feel managed or truly met, explained away or genuinely understood.
Within supportive spaces, this becomes an invitation to approach one another with compassion and curiosity. In practice, that can look like:
Supporting loved ones in seeking support: Encouraging and walking alongside friends or family members as they access neurodivergent-affirmative support.
Understanding social energy: Masking (the effort to present in ways that feel socially acceptable) requires significant mental energy and can be deeply draining. When that “social battery” runs out, what may appear as withdrawal is often simply the natural recovery needed after prolonged adapting.
Being a safe space: Social energy can be demanding to manage, and for AuDHD individuals it matters deeply to have people who feel like “safe spaces.” These are friends or family who offer unconditional acceptance, where there is no pressure to mask. In these spaces, energy can be conserved, authenticity can breathe, and connection feels restorative rather than draining.
Acknowledging sensory differences: Overstimulation from light, sound, or touch can be overwhelming for autistic individuals, while for those with ADHD the same stimuli may compete for attention. ADHD can also bring sensory-seeking tendencies such as craving movement, novelty, or stimulation rather than avoiding it. For AuDHD individuals, these patterns often overlap, blending sensitivity with seeking. When peers respond with understanding and compassion, it reduces feelings of alienation and makes space for recognising when a change of environment or support might be appreciated.
Letting go of assumptions: Not everyone’s experience will mirror a stereotype. AuDHD opens a window into the many possible ways ADHD and autism can coexist.
Honouring uniqueness: Accepting that the neurodivergent experience is not less valid than the neurotypical one, just different.
When we dismantle “shoulds” and assumptions, AuDHD becomes less about categories and more about embracing the richness of diverse perspectives and experiences.
Living with AuDHD can feel like navigating a world that speaks a different language. But therapy can become a place where your language is honoured and you don’t have to translate or tone yourself down.
When we recognise both autism and ADHD together through neurodivergent affirming support, we move away from the narrative of being “too much” or “not enough.” Instead, we find belonging.
AuDHD sits right in a paradox: a reminder that our minds don’t have to fit neatly into diagnostic shapes to be real, valid, or worthy of care.
Here at Leone Centre, we have many experienced therapists who can offer you that support whether in person in London or online.

Have you ever asked yourself, “Is it ADHD or autism?” Maybe you see traits of both and feel like no single diagnosis fully explains your experience. You’re not alone.
Autism and ADHD often occur together, a combination known as AuDHD. While research has long recognised the overlap between these two conditions, the concept of AuDHD is still relatively new in clinical settings. It’s also not yet widely understood or formally recognised in diagnostic manuals.
This lack of recognition can make it harder for people with AuDHD to find answers or receive a diagnosis that captures their experience. Many are left navigating years of confusion, misdiagnosis, and feeling misunderstood.
In this post, we’ll explore what AuDHD means, the key symptoms to look out for, and why getting the right diagnosis can make a big difference. By understanding the connection between autism and ADHD, you can begin to navigate life with more confidence, self-awareness, and compassion.
AuDHD is a term used when someone is diagnosed with both Autism Spectrum Condition (ASC) and Attention-Deficit Hyperactivity Disorder (ADHD). These are both neurodevelopmental conditions. This means autism and ADHD affect how the brain develops and works, especially in areas like communication, attention, and behaviour.
Research suggests a significant overlap: studies estimate that 30% to 80% of autistic children may also meet the criteria for ADHD, and that around 20% to 50% of children with ADHD meet the criteria for autism.
While each condition has its own set of traits, they can overlap in ways that make diagnosis tricky. Understanding how they interact is essential for getting the right support, whether for yourself, a loved one, or someone in your care.
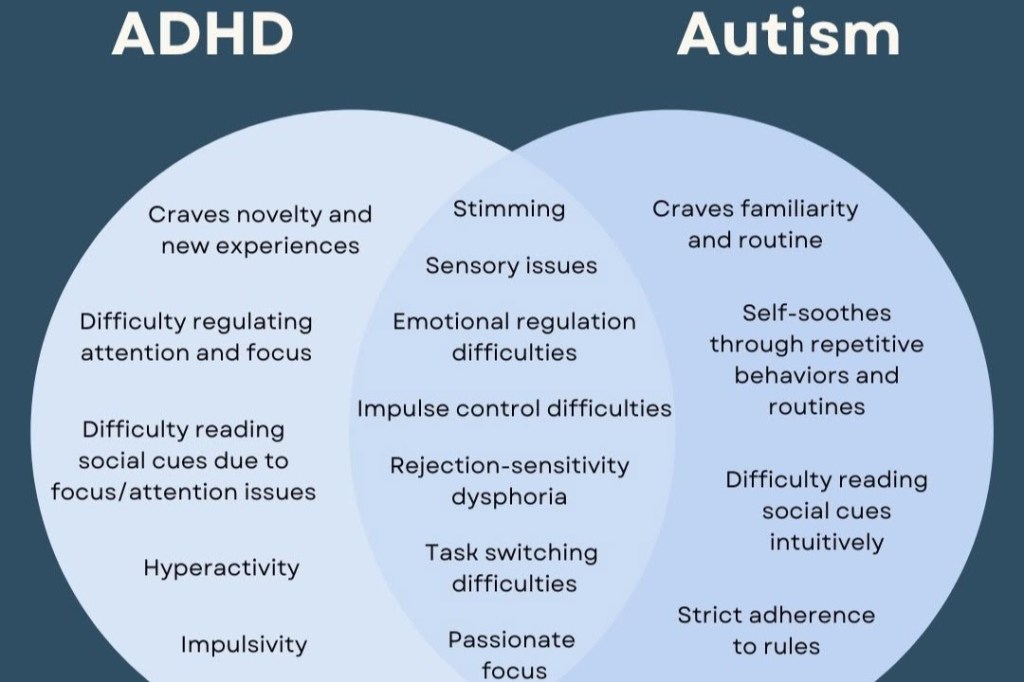
Although autism and ADHD are separate conditions, research shows they share some common ground. Both are linked to differences in brain development and neurotransmitter function, like dopamine. Particularly in brain regions involved in planning, organisation, emotional regulation, and sensory processing.
People with both autism and ADHD might:
Still, it’s important to note key differences. Autism typically affects how a person communicates and experiences the world. ADHD mainly impacts attention, restlessness, and impulse control.
No, ADHD is not a form of autism, but they do share similarities. They are recognised as distinct conditions with their own diagnostic criteria and neurological profiles.
For example, common symptoms of autism may include:
In contrast, core ADHD symptoms include:
ADHD often shows up differently in women and girls, which can lead to underdiagnosis or misdiagnosis. While boys may be disruptive or hyperactive, girls often internalise their struggles.
Common signs in women include:
This hidden presentation means many women don’t receive a diagnosis until adulthood. (You can read more about ADHD in women in our dedicated blog post.)
In kids, symptoms are usually more visible compared with adults. For example:
In adults, the signs are often more subtle. Hyperactivity may look like constant mental restlessness. Adults with autism might appear “socially competent” but only because they’ve learned to mask their traits. This often comes at a cost to their mental health.
When someone has autism and ADHD, these traits can interact in complicated ways. People with both autism and ADHD can experience a wide range of challenges that go beyond either condition alone. For example, someone might hyperfocus on a special interest (autistic trait) but still struggle to complete tasks due to distractibility (ADHD trait).
Here are some common AuDHD experiences:
Women with AuDHD often don’t match the typical (often male-based) diagnostic criteria. Instead of being outwardly hyperactive, they may:
Because their struggles are less visible, women are often overlooked or misdiagnosed. Sometimes with anxiety, depression, or personality disorders instead of the underlying neurodevelopmental conditions.
Recent research has drawn attention to this gender gap in diagnosis. For decades, neurodivergent women and girls have been left behind. Facing long waits, limited support, and a lack of recognition. As more women begin to identify with both ADHD and autism, it’s clear that we need more inclusive assessments and better understanding of how these conditions show up across genders.
Although autism and ADHD can look similar, their core differences matter:
The overlap between traits can be confusing. For example, difficulty focusing could be due to ADHD, or it could stem from autistic sensory overload. That’s why professional assessments are key to understanding the full picture.
If you’re unsure where to start, our psychiatrists can offer an initial consultation to decide whether to begin with an ADHD or autism assessment. Contact us to find out more.
AuDHD is not formally recognised as a condition in clinical guidelines like the DSM-5 or ICD-11. However, research and recognition of AuDHD is growing. More clinicians are starting to recognise that people diagnosed with both ADHD and autism require unique care. Clinicians may use a combination of evidence-based approaches to assess for autism and ADHD separately while considering how traits interact, such as:
Because symptoms of autism and ADHD can mimic or mask each other, it’s important to work with a clinician who understands both. They’ll look at how traits interact, not just how symptoms show up in isolation. For example, impulsive behaviour could be driven by ADHD, or it might be a sensory-seeking trait linked to autism.
If you suspect you have ADHD with autism, seeking a specialist familiar with both conditions is essential. You can explore more about ADHD assessments and the evaluation process here.
You can also begin with our free ADHD screening test for adults.
Assessment for autism and ADHD (AuDHD) often includes a clinical interview accompanied by questionnaires and information from people who know you well.
The assessment process may involve screening questionnaires such as the Autism Spectrum Quotient (AQ) and ADHD rating scales. Additionally, professionals may conduct direct behavioural observations and cognitive testing to assess attention regulation, impulsivity, and social interaction challenges. These tests help determine if an individual fits the profile of AuDHD and rule out other possible explanations for their symptoms.
If you’re considering an assessment, our team can support you through the process. Speak with our friendly medical secretaries today, and they can help match you with a clinician who specialises in both ADHD and autism.
Life with AuDHD can feel like a rollercoaster. Sometimes you might feel hyperfocused and energised, other times you can feel completely overwhelmed or shut down.
But understanding your brain can change everything. Studies show that people with autism are much more likely to also have ADHD, and vice versa people with ADHD are more likely to have autism. Yet many still go undiagnosed for years.
Knowing you have AuDHD helps you get the right support and make choices that actually work for you, instead of constantly trying to fit into a neurotypical mold.
People with ADHD and autism often face a unique set of hurdles in everyday life. Common challenges can include:
Despite the daily struggles, AuDHD individuals also bring exceptional strengths to the table. Their unique perspective often leads to creative problem-solving and out-of-the-box thinking. Having a deep focus and passion for specific interests often allows them to become experts in their field. Emotional sensitivity (often seen as a challenge) can also lead to a powerful form of empathy.
Understanding the difference between autism and ADHD can clarify how these strengths emerge differently. Recognising your unique abilities is as vital as acknowledging your struggles.
AuDHD burnout can be intense, prolonged, and deeply misunderstood. AuDHD burnout is beyond just feeling tired. It’s a deep physical and emotional crash caused by chronic stress and sensory/emotional overload. This kind of burnout arises from the effort of masking symptoms, managing autism and ADHD symptoms, and navigating a world not built for neurodivergent minds. Signs of burnout can include:
Recovery means more than just taking a break. It means making sustainable changes, like reducing demands, setting boundaries, and building a life that works with your brain, not against it.
Managing AuDHD starts with self-awareness. Once you understand how your traits show up, you can build systems that work for you.
Here are a few strategies that can help:
Most importantly, give yourself permission to do things differently. You’re not broken! Your brain just works differently.
There’s no “one-size-fits-all” approach, but many people with AuDHD benefit from:
At the London Psychiatry Clinic, we offer assessments and support tailored to people navigating both autism and ADHD. You can book an ADHD assessment or take a free adult ADHD test to get started.
Living with AuDHD can be complicated, but it doesn’t have to be confusing. With the right understanding, support, and tools, you can manage your challenges and celebrate your strengths.